Key takeaways:
- Ozempic and Wegovy may reduce cravings, but they do not resolve the underlying drivers of compulsive behaviour.
The emerging science suggests these medications dampen reward signals — they don’t retrain the nervous system. - Cravings are a symptom of nervous system dysregulation, not the core problem.
Alcohol, sugar and other compulsive behaviours are often attempts to regulate stress, overwhelm and emotional discomfort. - Lasting change comes from regulation, skills and structure — not medication alone.
Reduced cravings can create space, but sustainable recovery requires behavioural change, emotional regulation and lifestyle stability.
Medications like Ozempic and Wegovy are dominating headlines, not just for weight loss, but for their potential to reduce cravings for alcohol, sugar and other compulsive behaviours. At Noosa Confidential, we are paying close attention. The science is genuinely interesting, but it is also important to stay grounded in what we know, what we do not yet know, and what actually creates lasting change.
We are at the edge of emerging research, not the end point.
What the Research Is Suggesting (In Simple Terms)
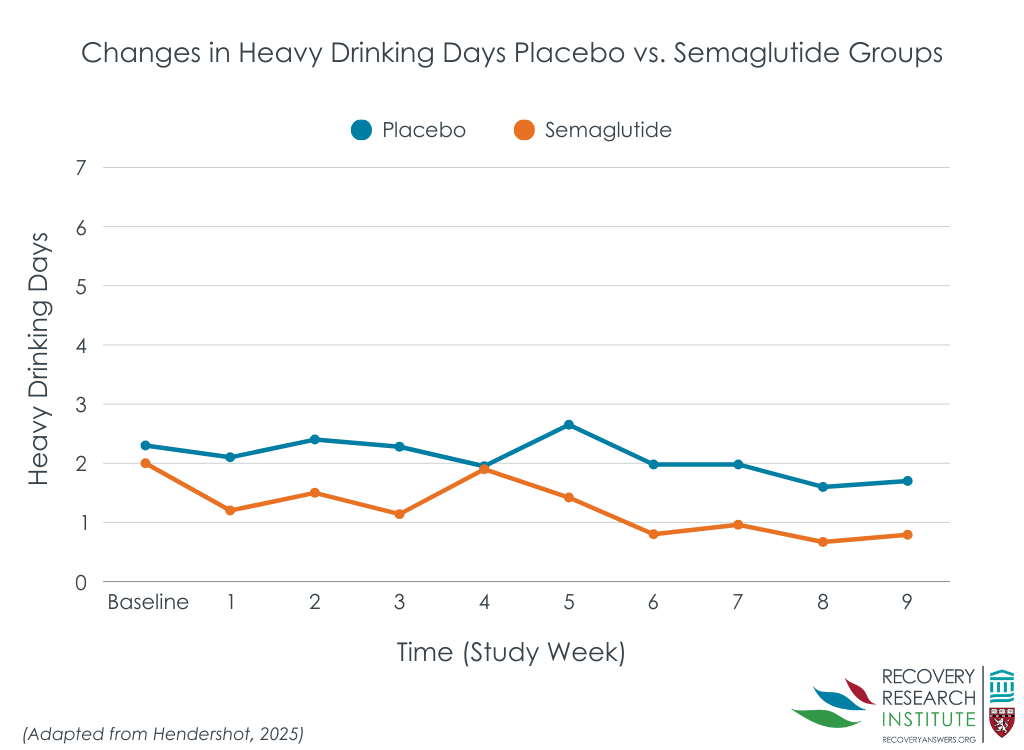
These medications work on the GLP-1 system, which influences appetite, satiety and parts of the brain involved in reward and motivation. Researchers are now observing that by dampening reward-seeking signals, these drugs may reduce the intensity of cravings, not only for food, but also for alcohol and sugar.
In practical terms, some people experience:
- Less urge to drink or binge
- Reduced desire for highly stimulating foods
- Fewer compulsive, dopamine-driven behaviours
That matters. For some individuals, reduced cravings can create space. A pause where better decisions become possible.
This is not unusual in medicine and makes sense. Many drugs are developed for one purpose and later found to be helpful for others, particularly when used thoughtfully and often at lower doses.
At Noosa Confidential, we already use this in practice. A current client uses naltrexone, a medication originally developed for opioid dependence that is now commonly used to reduce alcohol cravings by dampening the reward response.
It is unsurprising that Ozempic may reduce sugar and alcohol cravings, given alcohol is metabolised as sugar and engages the same reward circuits.
However, addiction is not simply a craving problem.
Why Treating Cravings isn't enough.
Cravings are not the root issue. They are a signal.
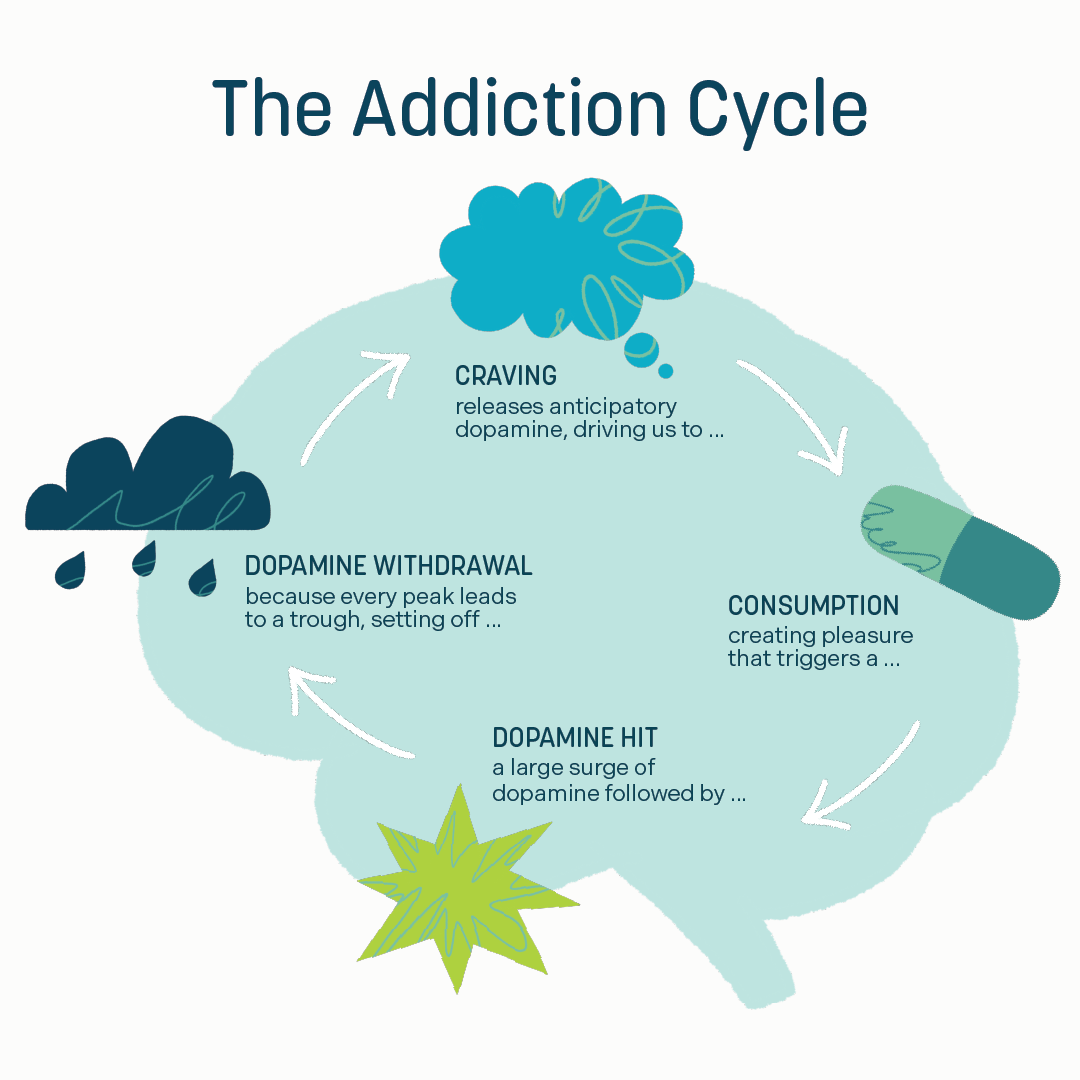
Most compulsive behaviours, whether alcohol, food, sugar, work or stimulation, are attempts to regulate an overwhelmed nervous system. They are ways the body tries to feel relief, calm or control when it does not know how to do that internally.
When the nervous system is chronically dysregulated:
- Stress remains high
- Dopamine becomes the coping strategy
- The body learns to rely on spikes rather than stability
Medication may turn the volume down on cravings, but it does not teach the system how to regulate itself. Without learning new skills, the underlying need for those behaviours remains.
The Risk of a Band-Aid Approach
This is where caution is needed.
If medication is used without addressing sleep, stress, emotional regulation, habits, mindset and lifestyle, it becomes a temporary fix. When the medication stops, or when life becomes demanding again, old patterns often return.
Long-term change does not come from suppressing symptoms. It comes from rewiring the system that created them.
What Actually Creates Sustainable Change
At Noosa Confidential, our focus is on treating the whole system, not just the behaviour.
That means:
- Regulating the nervous system rather than overriding it
- Reducing dependence on dopamine spikes
- Teaching skills for emotional regulation and distress tolerance
- Creating structure, rhythm and stability in daily life
- Addressing the psychological drivers behind compulsive patterns
When these foundations are in place, cravings lose their power. Not because they are blocked, but because they are no longer needed.
Medication can sometimes support this process. It may reduce intensity while someone learns new ways of responding. But medication is not the work. The work is learning how to live differently, in your body, your brain and your behaviour.
How Noosa Confidential is integrating emerging science — without chasing shortcuts
The research into GLP-1 medications and cravings is worth watching. It may become one useful tool within a broader, evidence-based treatment framework.
But it will never replace:
- Skill development
- Lifestyle change
- Nervous system regulation
- Psychological and behavioural work
There is no injection for resilience.
No pill for emotional regulation.
No shortcut to sustainable change.
That is why we continue to do what we do, grounded in science, focused on root causes, and committed to helping people build change that lasts.
The science:
- Sinha, B., Ghosal, S. The effects of glucagon-like peptide-1 receptor agonists (GLP1-RAs) on alcohol-related outcomes: a systematic review and meta-analysis. Addict Sci Clin Pract (2025). https://doi.org/10.1186/s13722-025-00637-z
- JAMA Psychiatry, Published Online: February 12, 2025: 2025;82;(4):395-405. doi:10.1001/jamapsychiatry.2024.4789
- Eshraghi R, Ghadimi DJ, Montazerinamin S, Bahrami A, Kachela Y, Rezasoltani M, Namazi MJ, Subhani M, Ebrahimi P, Hosseini K. Effects of glucagon-like peptide-1 receptor agonists on alcohol consumption: a systematic review and meta-analysis. EClinicalMedicine. 2025 Nov 14;90:103645. doi: 10.1016/j.eclinm.2025.103645. PMID: 41324012; PMCID: PMC12663662.
Find out more about how you can work with Noosa Confidential to implement long-term sustainable change.