Key takeaways:
- Food Shapes Mental Health
What we eat directly affects brain function, mood, cravings, and emotional regulation. Blood sugar instability, insulin resistance, and ultra-processed foods are now clearly linked to anxiety, depression, burnout, and addiction. - Metabolic and Gut Health Matter in Recovery
Stabilising blood sugar, reducing inflammation, and supporting gut health create the biological conditions needed for therapy and recovery to work. - Policy Is Catching Up to the Science
The new food pyramid reflects long-standing evidence: real food, healthy fats, and individual metabolic needs support brain health and sustainable mental wellbeing.
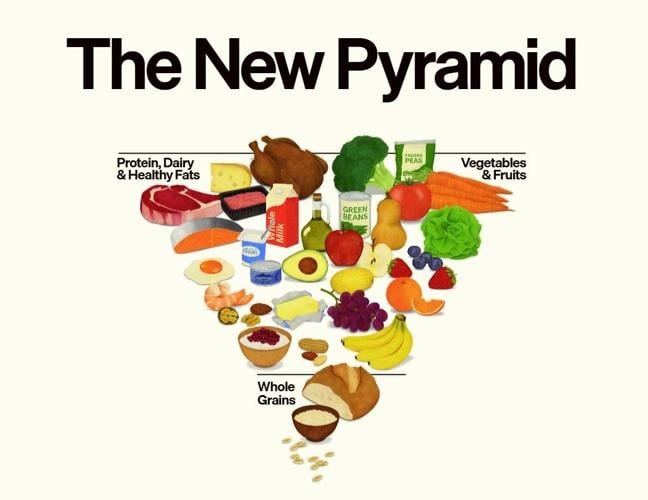
The recent changes to the US food pyramid aren’t just a nutrition update. They’re a quiet acknowledgement that decades of dietary advice haven’t delivered the health outcomes we were promised.
For years, guidelines focused on calories and weight. Fat was framed as the problem. Carbohydrates formed the base of the pyramid. Ultra-processed foods thrived as long as they met macronutrient targets. Over the same period, rates of insulin resistance, obesity, anxiety, depression, burnout, and addiction continued to rise.
That gap between advice (often shaped by commercial interests) and real-world outcomes is now too large to ignore.
At Noosa Confidential, this shift doesn’t surprise us. For more than 16 years, our programs have been guided by scientific research and clinical outcomes, with a strong focus on gut health and metabolic regulation. We’ve integrated lower-carbohydrate, whole-food, higher-fat nutrition not because it was fashionable, but because the evidence consistently shows it supports brain function and recovery.

These strategies may be simple, but they consistently deliver meaningful outcomes for our clients. Within as little as a week, we often see noticeable shifts in energy levels, improvements in digestion, and positive changes in mood. When combined with the other protocols we offer to support clients as a whole this builds momentum for good outcomes - Amanda Noosa Confidential's Head of Nutrition and GAPS qualified coach
Food Shapes the Brain First
Mental health doesn’t sit outside the body — it emerges from it.
Blood sugar instability, insulin resistance, and inflammation are strongly linked to:
- low mood
- anxiety
- cognitive impairment
- emotional reactivity.
Repeated glucose spikes activate stress pathways and cortisol, placing added strain on an already sensitised nervous system, particularly in people with trauma histories or addiction vulnerability.
Ultra-processed foods further drive inflammation, while whole-food diets that include adequate protein and healthy fats support metabolic stability, brain function, and steadier mood.
Fats provide reliable fuel for the brain and support hormone balance and satiety, while protein supplies the building blocks for neurotransmitters that regulate mood, motivation, focus, and stress.
Together, they stabilise blood sugar, reduce irritability and cravings, and support emotional regulation - outcomes that are critical during hormonal or metabolic disruption, and especially in addiction recovery and detox, where nutrient depletion and unstable physiology can intensify anxiety, emotional volatility, and compulsive behaviour.
The American Guidelines state HERE:
We are putting real food back at the center of the American diet. Real food that nourishes the body. Real food that restores health. Real food that fuels energy and encourages movement and exercise. Real food that builds strength. (
This Isn’t New — It Was Just Ahead of Policy
Long before governments began revisiting dietary guidelines, clinicians were already observing these effects.
- Dr Terry Wahls demonstrated how targeted nutrition could influence neurological and autoimmune conditions by reducing inflammation and supporting mitochondrial function.
- Dr Natasha Campbell-McBride highlighted the gut–brain axis, aligning with research now showing links between gut inflammation, microbiome imbalance, and psychiatric symptoms (Psychiatry Research, Cell).
This work sits within the growing field of nutritional psychiatry, which examines how diet influences neurotransmitters, inflammation, stress pathways, and addiction vulnerability.
What the New Pyramid Really Signals
The updated food pyramid reflects a broader move away from one-size-fits-all advice and toward real food, metabolic health, and individual response. That’s a meaningful shift.
The challenge now is ensuring this knowledge moves beyond policy documents and into schools, healthcare, and everyday understanding. Because food has always influenced how we feel, cope, and recover — the science is simply making that harder to deny.
At Noosa Confidential, nutrition is never the whole answer. But when food supports the nervous system instead of overwhelming it, everything else has a better chance of holding.
The Science
Horn J, Mayer DE, Chen S, Mayer EA. Role of diet and its effects on the gut microbiome in the pathophysiology of mental disorders. Transl Psychiatry. 2022 Apr 20;12(1):164. doi: 10.1038/s41398-022-01922-0. PMID: 35443740; PMCID: PMC9021202
Penckofer S, Quinn L, Byrn M, Ferrans C, Miller M, Strange P. Does glycemic variability impact mood and quality of life? Diabetes Technol Ther. 2012 Apr;14(4):303-10. doi: 10.1089/dia.2011.0191. Epub 2012 Feb 10. PMID: 22324383; PMCID: PMC3317401.
Wang CB, Tang J, Cao Y. Feeding the mood: The role of macronutrients in depression prevention and treatment. World J Psychiatry. 2025 Aug 19;15(8):107435. doi: 10.5498/wjp.v15.i8.107435. PMID: 40837787; PMCID: PMC12362651.

.webp)
